Over the last three decades, the number of mobile health clinics operating in the U.S. has grown exponentially. These doctors’ offices on wheels are an essential part of the healthcare system, numbering approximately 3,000 across the nation. The care they deliver is crucial, even life-saving, and the units often provide access to a range of healthcare services in one place, from pediatric care, behavioral health, and cancer screening. Read on to learn how mobile health care meets the needs of Americans in big cities and rural areas alike.
In 2020, COVID-19 quickly became a public health crisis that required different approaches to healthcare delivery. Because mobile clinics supported care outside traditional hospital and clinic settings, countless community health systems across the country relied upon them to see millions of patients and support pandemic recovery efforts. Today, many of those mobile clinics have been converted from triage, testing and vaccination stations to full-service community health centers.
The rise in opioid-related health problems has also drawn attention to the advantages of mobile healthcare, especially for substance use disorder treatment and harm reduction. In 2019, the U.S. Drug Enforcement Agency amended its regulations making it easier to provide methadone treatment on mobile units. In addition, a growing number of clinics prescribe other medications to help people trying to stop using opioids, distribute naloxone to help reverse overdoses, and offer clean needle exchange, fentanyl testing, and wound care. California recently announced grant opportunities for organizations aiming to start mobile addiction programs. Other states are likely to follow suit as new funding becomes available through opioid settlement funds.
The growth is also fueled by research that supports the practice of mobile healthcare. Dr. Nancy Oriol’s 2009 paper, Calculating the return on investment of a mobile clinic, sparked new interest among health care leaders, funders, and researchers.
And today, research demonstrates that mobile clinics improve health outcomes through screenings, preventative care, and chronic disease management. They can help communities lower pre-term birth rates, manage hypertension, and encourage self-efficacy in patients. Mobile clinics also address social determinants of health by providing medical care alongside broader social services, and they make economic sense.
The current field has been supported by a combination of philanthropy, federal and state funding, insurance reimbursement, and patient payments. These funding streams, however, are unpredictable and inefficient.
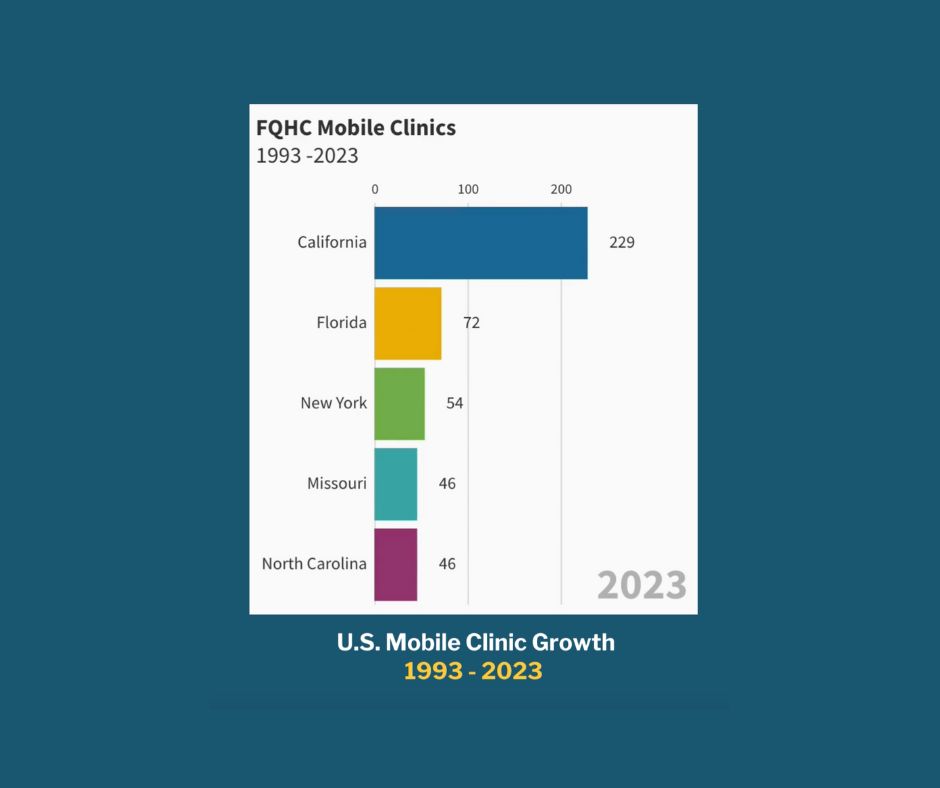
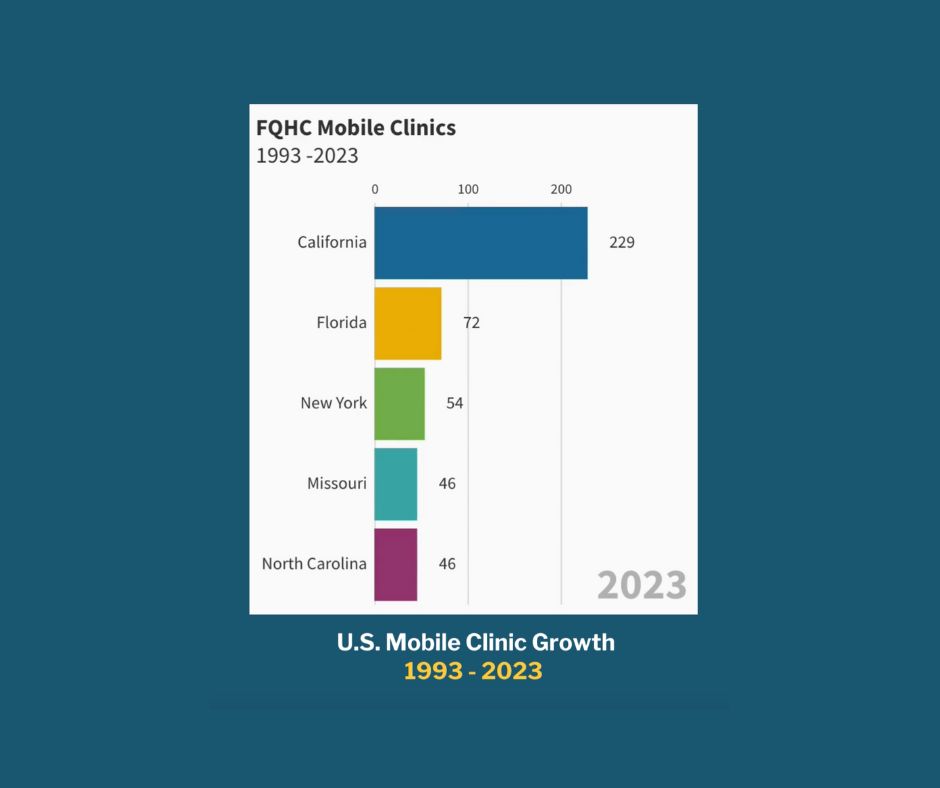
Federally-qualified community health centers (FQHCs), unlike most other organizations that operate mobile clinics, are better positioned to sustain their mobile programs because they receive enhanced reimbursement under Medicare and Medicaid. They also serve populations that most likely to benefit from the convenience, flexibility, and accessibility of this care delivery model. FQHCs will likely continue contributing to the growth of the sector thanks to the MOBILE Health Care Act passed in 2023. This bipartisan legislation enables FQHCs to use New Access Points Grants for establishing mobile clinics without also creating a new fixed site.
Clearly, we can make the case for how mobile health care meets the needs of Americans:
During a time when confidence in the healthcare system is at an all-time low, mobile health providers build trust and community partnerships. They contribute to a more equitable healthcare system.
As we continue to understand their impact and potential, it’s essential to support their integration into the broader healthcare infrastructure.
To learn more about the mobile clinics in communities across the nation, check out our interactive mobile clinic impact tracker.
Mollie Williams, MPH, DrPH is Executive Director of The Family Van and Mobile Health Map and Lecturer of Global Health and Social Medicine at Harvard Medical School. In her free time, she enjoys spending time with her family, traveling, and textile arts.